Ocular bobbing, dipping and floating are not too rare, if you keep examining your comatose and brainstem patients repeatedly. We discuss the few things that are known about these eye movement disorders and relish the wonderful poem of Ross 1992:
You’re called to the bedside, the eye movements are strange.
There must be a reason, can you give it a name?
You’ve seen this before, but can you recall?
You’re the Neurologist, you’re supposed to know all!
In bobbing and dipping, the eyes go down.
“How is that?” you ask with a frown.
The first is brisk, the second is slow.
The meaning differs; you must know.
Bobbing suggest pons; dipping an anoxic brain.
As always, there are some exceptions to name.
Metabolic encephalopathy can make the eyes bob.
Cerebellar hemorrhage and trauma complete the log.
To remember all this, you need something terse.
But wait, don’t forget, it could be reverse!
In each of these cases, it’s up the eyes go.
Bobbing is fast and dipping is slow.
Reverse bobbing may be something you see,
again, with metabolic encephalopathy.
Reverse dipping, a rare clinical nidus,
is reported in AIDS with cryptococcal meningitis.
Despite the confusion, one thing is plain.
The eyes don’t work right, whatever the name.
Wheter bobbing or dipping or reversing is true,
it can’t be good; just be glad it’s not you!
I would add that in Bobbing usually the horizontal VOR fails (with calorics or doll’s head maneuver). Here is a link to an article about the stuff
The clinical spectrum of ocular bobbing and ocular dipping. JNNP 1988.
Showing posts with label Ophthalmoplegia. Show all posts
Showing posts with label Ophthalmoplegia. Show all posts
Saturday, July 19, 2014
Thursday, January 17, 2013
Bilateral Internuclear Ophthalmoplegia in Multiple Sclerosis
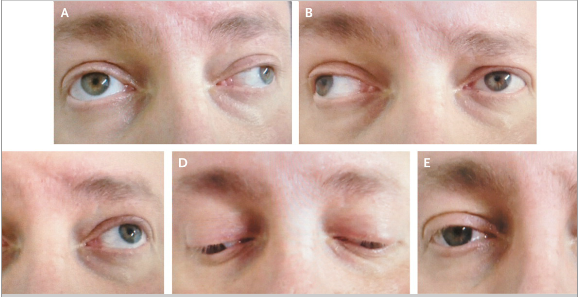
A 45-year-old man with multiple sclerosis presented with worsening
weakness in his right leg and double vision. Neurologic examination
revealed horizontal diplopia during lateral gaze in both eyes. The
patient had an adduction deficit in the right eye and nystagmus in the
left eye on leftward gaze (Panel A). He also had an adduction deficit in
the left eye and nystagmus in the right eye on rightward gaze (Panel
B). Upward gaze (Panel C), downward gaze (Panel D), and normal primary
position (Panel E) were unremarkable.
Internuclear ophthalmoplegia is characterized by impaired horizontal
eye movement that is caused by a lesion in the medial longitudinal
fasciculus, a fiber tract that rises from the abducens nucleus in the
pons to the contralateral oculomotor nucleus in the midbrain. Lesions in
the medial longitudinal fasciculus result in the failure of adduction
on attempted lateral gaze. Any brain-stem syndrome can interrupt the
medial longitudinal fasciculus and result in impaired horizontal eye
movement, but the most frequent underlying cause is multiple sclerosis.
This patient had internuclear ophthalmoplegia in both eyes due to
demyelinating lesions. Glucocorticoids were administered intravenously,
but the deficits did not resolve. On follow-up at 2 months, the
patient's gait had improved, but the internuclear ophthalmoplegia
remained.
Subscribe to:
Posts (Atom)