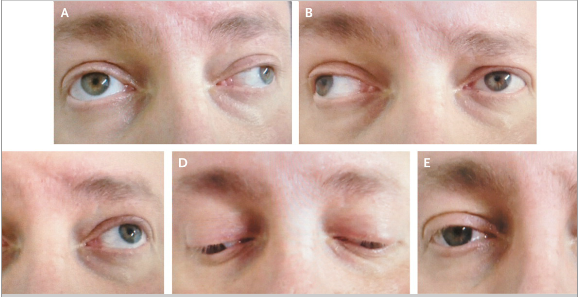
A 45-year-old man with multiple sclerosis presented with worsening
weakness in his right leg and double vision. Neurologic examination
revealed horizontal diplopia during lateral gaze in both eyes. The
patient had an adduction deficit in the right eye and nystagmus in the
left eye on leftward gaze (Panel A). He also had an adduction deficit in
the left eye and nystagmus in the right eye on rightward gaze (Panel
B). Upward gaze (Panel C), downward gaze (Panel D), and normal primary
position (Panel E) were unremarkable.
Internuclear ophthalmoplegia is characterized by impaired horizontal
eye movement that is caused by a lesion in the medial longitudinal
fasciculus, a fiber tract that rises from the abducens nucleus in the
pons to the contralateral oculomotor nucleus in the midbrain. Lesions in
the medial longitudinal fasciculus result in the failure of adduction
on attempted lateral gaze. Any brain-stem syndrome can interrupt the
medial longitudinal fasciculus and result in impaired horizontal eye
movement, but the most frequent underlying cause is multiple sclerosis.
This patient had internuclear ophthalmoplegia in both eyes due to
demyelinating lesions. Glucocorticoids were administered intravenously,
but the deficits did not resolve. On follow-up at 2 months, the
patient's gait had improved, but the internuclear ophthalmoplegia
remained.