Saturday, October 12, 2013
Medical Research Council (MRC) Scale for Muscle Strength
The patient's effort is graded on a scale of 0-5:
Grade 5: Muscle contracts normally against full resistance.
Grade 4: Muscle strength is reduced but muscle contraction can still move joint against resistance.
Grade 3: Muscle strength is further reduced such that the joint can be moved only against gravity with the examiner's resistance completely removed. As an example, the elbow can be moved from full extension to full flexion starting with the arm hanging down at the side.
Grade 2: Muscle can move only if the resistance of gravity is removed. As an example, the elbow can be fully flexed only if the arm is maintained in a horizontal plane.
Grade 1: Only a trace or flicker of movement is seen or felt in the muscle or fasciculations are observed in the muscle.
Grade 0: No movement is observed.
Clinical grading scale employed for functional assessments
Grade 0: normal.
Grade 1: no disability; minor sensory signs or areflexia.
Grade 2: mild disability; ambulatory for >200 m; mild weakness in one or more limbs and sensory impairment.
Grade 3: moderate disability; ambulatory for >50 m without stick; moderate weakness MRC Grade 4 and sensory impairment.
Grade 4: severe disability; able to walk >10 m with support of stick; motor weakness MRC Grade 4 and sensory impairment.
Grade 5: requires support to walk 5 m; marked motor and sensory signs.
Grade 6: cannot walk 5 m, able to stand unsupported and able to transfer to wheelchair, able to feed independently.
Grade 7: bedridden, severe quadriparesis; maximum strength MRC grade 3.
Grade 8: respirator and/or severe quadriparesis; maximum strength MRC grade 2.
Grade 9: respirator and quadriplegia.
Grade 10: dead.
Reference:
Medical Research Council. Aids to the examination of the peripheral nervous system, Memorandum no. 45, Her Majesty's Stationery Office, London, 1981.
Hahn AF, Bolton CF, Pillay N, et al. Plasma exchange therapy in chronic inflammatory
demyelinating polyneuropathy. A double-blind, sham controlled, cross-over study.
Brain 1996;119:1055–66. [Medline]
Paternostro-Sluga T, Grim-Stieger M, Posch M, Schuhfried O, Vacariu G, Mittermaier C, Bittner C, Fialka-Moser V. Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J Rehabil Med. 2008 Aug;40(8):665-71.
Saturday, April 27, 2013
Tuesday, March 26, 2013
Thursday, January 17, 2013
Bilateral Internuclear Ophthalmoplegia in Multiple Sclerosis
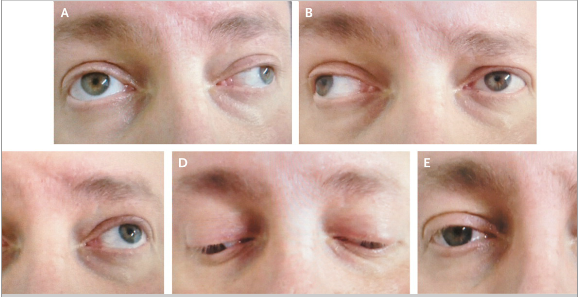
A 45-year-old man with multiple sclerosis presented with worsening
weakness in his right leg and double vision. Neurologic examination
revealed horizontal diplopia during lateral gaze in both eyes. The
patient had an adduction deficit in the right eye and nystagmus in the
left eye on leftward gaze (Panel A). He also had an adduction deficit in
the left eye and nystagmus in the right eye on rightward gaze (Panel
B). Upward gaze (Panel C), downward gaze (Panel D), and normal primary
position (Panel E) were unremarkable.
Internuclear ophthalmoplegia is characterized by impaired horizontal
eye movement that is caused by a lesion in the medial longitudinal
fasciculus, a fiber tract that rises from the abducens nucleus in the
pons to the contralateral oculomotor nucleus in the midbrain. Lesions in
the medial longitudinal fasciculus result in the failure of adduction
on attempted lateral gaze. Any brain-stem syndrome can interrupt the
medial longitudinal fasciculus and result in impaired horizontal eye
movement, but the most frequent underlying cause is multiple sclerosis.
This patient had internuclear ophthalmoplegia in both eyes due to
demyelinating lesions. Glucocorticoids were administered intravenously,
but the deficits did not resolve. On follow-up at 2 months, the
patient's gait had improved, but the internuclear ophthalmoplegia
remained.
Subscribe to:
Comments (Atom)